How Self-Expanding Stents Enhance Vascular and Coronary Interventions

Self-expanding stents have revolutionized vascular and coronary interventions by adapting to complex anatomical structures with precision. Their flexibility and chronic outward force allow them to conform seamlessly to irregular vessel shapes, minimizing trauma and promoting better healing. For instance, nitinol-based designs, such as the Devax coronary bifurcation system, demonstrate superior adaptability to non-tubular vascular structures, addressing challenges where conventional stents often fall short. Studies also reveal that self-expanding stents significantly reduce vascular injury within 30 days compared to balloon-expandable alternatives, enhancing procedural success and long-term outcomes. These advancements mark a pivotal shift in coronary care.
Key Takeaways
Self-expanding stents fit different vessel shapes, causing less damage and helping healing.
Constant outward pressure keeps vessels open, reducing risks like re-narrowing.
Nitinol's special features make stents strong and bendable for tough cases.
Studies prove self-expanding stents lower re-narrowing and improve long-term results.
Skilled operators are key to placing stents safely and effectively.
Key Features of Self-Expanding Stents

Chronic Outward Force
Chronic outward force (COF) is a defining characteristic of self-expanding stents. This radial force ensures the stent maintains vessel patency by exerting consistent pressure against the arterial walls. Unlike balloon-expandable stents, self-expanding stents adapt to vessel dynamics, reducing the risk of restenosis and vessel trauma. For example, the Supera™ Stent demonstrates superior performance with minimal COF, significantly lowering vessel injury rates. Its unique design, which matches the vessel diameter 1:1, minimizes endovascular damage over time.
Specification/Metric | Description |
|---|---|
Chronic Outward Force (COF) | The radial force exerted by the stent, influenced by design, strut thickness, and material properties. |
Compression Resistance | The Supera™ Stent exhibits over four times the compression resistance of other nitinol stents. |
These metrics highlight how COF contributes to procedural success and long-term outcomes in vascular interventions.
Strut Thickness and Flexibility
Strut thickness plays a critical role in the performance of self-expanding stents. Thinner struts reduce vascular injury and improve flexibility, allowing the stent to conform to complex vessel anatomies. Research shows that arteries treated with thick-strut stents experience higher rates of restenosis due to increased myointimal thickening. Maintaining an intact internal elastic lamina (IEL) is essential for preventing restenosis, making low-profile struts a priority in stent design.
Flexibility further enhances the adaptability of self-expanding stents. This feature ensures optimal deployment in tortuous vessels, reducing the risk of malapposition. The Pulsar-18 stent, with its 140 µm struts, exemplifies this balance between flexibility and durability, achieving a lower metal-to-artery ratio while maintaining structural integrity.
Material Composition and Durability
The material composition of self-expanding stents directly impacts their durability and performance. Nitinol, a nickel-titanium alloy, is the material of choice due to its super-elasticity and biocompatibility. This unique property allows the stent to recover its shape after deformation, minimizing vessel wall injury and supporting long-term durability. The nearly equiatomic composition of nitinol enhances its mechanical properties, ensuring the stent withstands various stresses.
Nitinol's crystalline phases (martensite and austenite) can be controlled during production, optimizing chronic outward force and flexibility.
The Pulsar-18 stent's thin struts and low fracture rates demonstrate the durability of nitinol-based designs, even in challenging anatomical locations.
The STENTYS® stent, with its memory diameter exceeding vessel size, adapts automatically, enhancing its performance over time.
These features make nitinol-based self-expanding stents, such as those offered by AccuPath, indispensable in modern vascular care.
Clinical Evidence for Self-Expanding Stents
Reduced Restenosis Rates
Self-expanding stents have demonstrated remarkable efficacy in reducing restenosis rates, particularly in challenging cases like femoropopliteal artery disease. Their ability to conform to vessel anatomy minimizes vascular injury, which is a key factor in restenosis prevention. Clinical studies, such as the DIVERGE IVUS substudy, reported a stent thrombosis rate of just 1% at nine months, showcasing their reliability. Furthermore, trials like XAMI and COMFORTABLE-AMI revealed one-year recurrent myocardial infarction (MI) rates as low as 0.5%, further emphasizing their role in improving coronary outcomes.
Study | Outcome | Result |
|---|---|---|
DIVERGE IVUS substudy | Stent thrombosis rate at 9 months | 1% |
XAMI, COMFORTABLE-AMI, EXAMINATION trials | One-year recurrent MI rates | 0.5%-3.7% |
These findings highlight the potential of self-expanding stents in reducing restenosis and improving primary patency in coronary and vascular interventions.
Long-Term Outcomes in Vascular and Coronary Interventions
Long-term follow-up data underscores the durability and effectiveness of self-expanding stents. Patients treated with these stents experience significantly less vascular injury at 30 days compared to balloon-expandable alternatives. By 180 days, injury scores become comparable, indicating sustained vessel healing. In cases of myocardial infarction or heart failure, self-expanding stents reduce restenosis risks, often caused by undersized stents in these scenarios. Additionally, trials suggest lower rates of target lesion revascularization in saphenous vein grafts, further validating their long-term clinical outcomes.
Self-expanding stents reduce vascular injury at 30 days, with comparable scores by 180 days.
They lower restenosis risks in myocardial infarction and heart failure patients.
Trials indicate reduced target lesion revascularization rates in saphenous vein grafts.
These outcomes demonstrate the superiority of self-expanding stents in the treatment of femoropopliteal occlusive disease and other complex conditions.
Performance of Specific Stent Models
Specific self-expanding stent models, such as the STENTYS and AXXESS, have shown exceptional performance in clinical studies. The STENTYS stent, for instance, achieved a stent thrombosis rate of 1.3% with post-dilatation, compared to 3.6% without it. Additionally, it exhibited lower malapposition rates (0.58%) compared to balloon-expandable stents (5.46%). The AXXESS stent demonstrated a 1% thrombosis rate at nine months, further solidifying its reliability.
Stent Model | Stent Thrombosis Rate | MACE Rate | Additional Notes |
|---|---|---|---|
STENTYS | 3.6% (without post-dilatation) | 3.6% (without post-dilatation) | Lower stent malapposition compared to balloon-expandable group (0.58% vs 5.46%) |
AXXESS | 1% at 9 months | N/A | Good results in stent thrombosis and target lesion revascularization at 6-month follow-up |
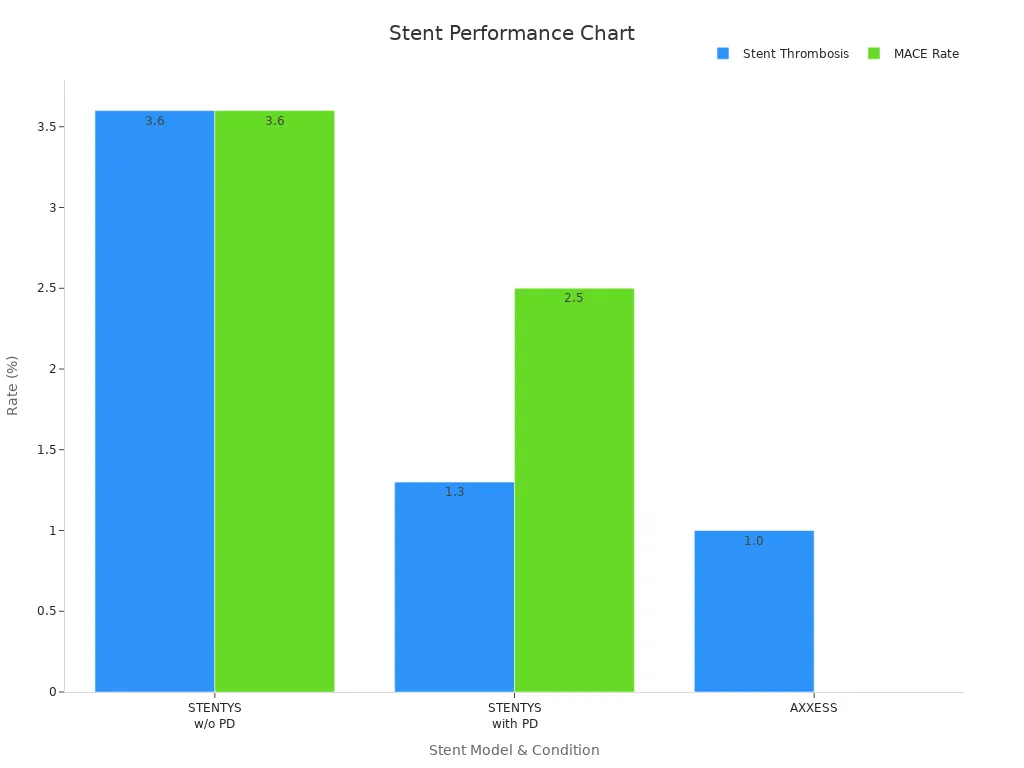
These models exemplify the advancements in self-expanding stent technology, offering improved clinical outcomes and primary patency in coronary and vascular interventions.
Challenges and Considerations in Using Self-Expanding Stents
Avoiding Oversizing and Vessel Damage
Oversizing remains a critical challenge in the clinical use of self-expanding stents. Studies reveal that oversized stents can lead to increased vessel wall injury and luminal area stenosis. This correlation between the stent-to-artery ratio and stenosis highlights the importance of precise sizing. Stents with low chronic outward force (COF) and thin strut designs, such as those offered by AccuPath, minimize vessel trauma while maintaining safety and efficacy. Animal studies further demonstrate that reducing oversizing significantly lowers the risk of restenosis, ensuring better long-term outcomes.
Evidence Type | Description |
|---|---|
Stent Design Impact | Low COF and thin struts reduce vessel wall injury and restenosis rates. |
Oversizing Effects | Oversized stents increase injury and luminal stenosis, compromising safety. |
These findings underscore the need for careful stent selection and deployment techniques to enhance procedural safety.
Patient-Specific Factors in Stent Selection
Patient-specific anatomical and clinical factors play a pivotal role in stent selection. Large, ectatic, or aneurysmal vessels, as well as tapered or vasoconstricted arteries, present unique challenges. For instance, patients with STEMI or chronic total occlusions often exhibit vasoconstriction due to elevated thrombus burden. This condition increases the likelihood of undersized stents, which are associated with higher restenosis rates. Self-expanding stents, like those made from nitinol, adapt to these anatomical complexities, providing superior outcomes in the treatment of femoropopliteal occlusive disease.
In myocardial infarction cases, self-expanding stents offer a distinct advantage. Their ability to conform to vessel dynamics ensures better wall apposition, reducing complications such as stent thrombosis. This adaptability makes them a preferred choice for complex coronary artery disease scenarios.
Importance of Operator Expertise
Operator expertise significantly influences the success of self-expanding stent procedures. Proper deployment techniques are essential to avoid complications like no-reflow or distal embolization, particularly in vessels with a high thrombus burden. Experienced operators can optimize stent sizing and placement, ensuring safety and efficacy. Training programs focusing on advanced stent technologies, such as AccuPath's nitinol-based designs, equip clinicians with the skills needed to navigate complex vascular cases.
Challenge Type | Description |
|---|---|
Stent Sizing | Issues in large or tapered vessels and vasoconstricted arteries. |
Complications | Higher MACE and stent thrombosis rates in STEMI patients. |
No-Reflow | Greater incidence in vessels with large thrombus burden. |
By addressing these challenges, operators can maximize the benefits of self-expanding stents, ensuring optimal outcomes for patients.
Advantages of Self-Expanding Stents

Enhanced Procedural Success
Self-expanding stents have demonstrated remarkable procedural success in both vascular and coronary interventions. Their ability to conform to vessel anatomy ensures optimal deployment, reducing complications such as malapposition and restenosis. Clinical studies, including the TASC D II Study and the PEACE Trial, have reported high primary patency rates of 85.4% and 79.5%, respectively, at 12 months. Freedom from target lesion revascularization (TLR) rates also exceeded 80% in these trials, underscoring their safety and efficacy.
Study Name | Primary Patency Rate (12 months) | Freedom from TLR Rate (12 months) |
|---|---|---|
TASC D II Study | 85.4% | 87.5% |
PEACE Trial | 79.5% | 81% |
BIOFLEX PEACE | 78% | 92.4% |
These results highlight the reliability of self-expanding stents in achieving procedural success, particularly in challenging cases like femoropopliteal artery disease.
Long-Term Clinical Benefits
The long-term clinical outcomes of self-expanding stents further validate their role in modern vascular care. These stents induce less vascular injury during implantation, promoting better healing and reducing the risk of restenosis. Their continuous expansion post-implantation ensures an optimal fit, enhancing vessel wall apposition and minimizing complications. A comparative analysis revealed that self-expanding stents outperform balloon-expandable alternatives in maintaining primary patency over extended periods.
Advantage | Description |
|---|---|
Reduced vascular injury | Self-expanding stents induce less injury at implantation, leading to better healing outcomes. |
Improved vessel wall apposition | They achieve better apposition, minimizing the risk of stent malapposition. |
Continuous enlargement | These stents continue to expand post-implantation, ensuring optimal fit and reducing restenosis. |
AccuPath's nitinol-based designs exemplify these benefits, offering superior safety and efficacy in the treatment of femoropopliteal occlusive disease.
Versatility in Treating Complex Cases
The versatility of self-expanding stents makes them indispensable in treating complex vascular and coronary conditions. Their self-apposing design adapts seamlessly to ectatic, tapered, or aneurysmal vessels, ensuring consistent apposition and reducing the risk of malapposition. The STENTYS self-expanding stent, for example, can expand beyond its indicated range, accommodating vessels up to 6.0 mm in diameter without additional treatment. This adaptability proves invaluable in scenarios involving large thrombus burdens or irregular vessel geometries.
Feature | Description |
|---|---|
Stent Type | STENTYS self-expanding stent |
Application | Used in ectatic, tapered, or aneurysmal vessels |
Design Advantage | Self-apposing design allows for apposition along the vessel, avoiding malapposition |
Expansion Capability | Can expand beyond indicated range for tapered or ectatic vessels |
Diameter Range | Indicated for vessels from 3.5 to 4.5 mm, can be used up to 6.0 mm without additional treatment |
AccuPath's nitinol tubing technology enhances this versatility, ensuring optimal clinical outcomes even in the most challenging cases.
Self-expanding stents have transformed vascular and coronary interventions by delivering superior clinical outcomes. Their ability to induce less injury during implantation and achieve better vessel wall apposition ensures enhanced safety and long-term success. For instance, the APPOSITION trials demonstrated that the STENTYS stent achieved a malapposition rate of only 0.58%, significantly outperforming balloon-expandable stents. Additionally, newer-generation nitinol stents with thinner struts improve deliverability and reduce in-stent restenosis, further enhancing primary patency rates.
Evidence Description | Outcome |
|---|---|
Self-expanding stents improve clinical outcomes by inducing less injury at implantation and achieving better vessel wall apposition. | Less injury at 30 days compared to balloon-expandable stents. |
The APPOSITION trials showed that the STENTYS self-expanding stent had significantly lower stent malapposition compared to balloon-expandable stents. | 0.58% malapposition vs. 5.46% in balloon-expandable group. |
Newer-generation self-expanding nitinol stents have thinner struts, improving deliverability and reducing in-stent restenosis. | Decreased rates of restenosis. |
While challenges like precise sizing and operator expertise remain, the advantages of self-expanding stents far outweigh these limitations. Their unique design and proven clinical performance make them indispensable in treating complex coronary cases. By ensuring better primary patency and reducing complications, these stents continue to redefine modern vascular care.
FAQ
What is a self-expanding stent, and how does it work?
A self-expanding stent is a medical device made from materials like nitinol. It expands automatically upon deployment, conforming to the vessel's shape. This adaptability ensures optimal vessel support and reduces complications such as restenosis, making it ideal for complex vascular and coronary interventions.
Why is nitinol commonly used in self-expanding stents?
Nitinol is preferred for its super-elasticity and biocompatibility. These properties allow the stent to recover its shape after deformation, ensuring durability and reducing vessel trauma. AccuPath's nitinol tubing technology exemplifies these advantages, offering reliable performance in challenging anatomical conditions.
How do self-expanding stents reduce restenosis rates?
Self-expanding stents conform to vessel anatomy, minimizing vascular injury during implantation. This reduces inflammation and myointimal thickening, key contributors to restenosis. Clinical studies consistently show lower restenosis rates with self-expanding stents compared to balloon-expandable alternatives.
What makes self-expanding stents suitable for complex cases?
Their flexibility and chronic outward force allow self-expanding stents to adapt to irregular vessel geometries. This versatility makes them effective in treating conditions like femoropopliteal artery disease or tapered vessels. Models like AccuPath's nitinol-based stents demonstrate exceptional adaptability and durability in such scenarios.
Are there any challenges in using self-expanding stents?
Challenges include precise sizing and operator expertise. Oversized stents can cause vessel damage, while undersized ones may lead to malapposition. Proper training and advanced stent designs, such as those offered by AccuPath, help mitigate these risks and ensure procedural success.

