Understanding Nitinol Stents for Arterial Disease Treatment

Nitinol stents for arterial diseases are innovative medical devices crafted from a nickel-titanium alloy known for its remarkable properties. These stents play a critical role in treating arterial diseases by restoring proper blood flow in blocked or narrowed blood vessels. Peripheral Artery Disease (PAD), a common condition causing restricted blood circulation, often benefits from the use of nitinol stents for arterial diseases. Their unique ability to adapt to vascular movements while maintaining durability makes them a preferred choice in modern interventions. Studies, such as those by Kickuth et al. (2007), have demonstrated a significant improvement in blood flow and patient outcomes, with a 6-month cumulative patency rate of 82% and enhanced resting ABI scores.
Key Takeaways
Nitinol stents are made from a nickel-titanium metal mix.
This metal lets the stents move with the body easily.
They are great for treating artery problems in the body.
These stents need only small cuts, so healing is faster.
Patients feel less pain and recover quicker than with surgery.
Nitinol stents help blood flow better and ease leg pain.
They also improve how patients feel and live every day.
Using these stents early can stop big problems like infections.
They can even prevent losing a limb from artery disease.
More doctors use nitinol stents because they work so well.
People want safer and easier treatments, so demand is growing.
Understanding Peripheral Artery Disease (PAD)
Causes and risk factors of PAD
Peripheral arterial disease occurs when arteries narrow due to plaque buildup, reducing blood flow to the limbs. Several factors contribute to its development:
Age: The risk increases significantly with age.
Smoking: Tobacco use damages blood vessels and accelerates plaque formation.
Hypertension: High blood pressure puts extra strain on artery walls.
Diabetes: Elevated blood sugar levels can harm blood vessels over time.
High cholesterol: Excess cholesterol contributes to plaque buildup.
Globally, the prevalence of peripheral arterial disease has risen dramatically. Between 1990 and 2019, the number of affected individuals increased by 72%, reaching over 113 million. Approximately 236 million people aged 25 and older live with this condition, with the majority residing in low- and middle-income countries. Women often experience a higher burden of disability, while men face greater mortality rates.
Symptoms and complications of PAD
Peripheral arterial disease often begins silently, with many individuals unaware of their condition. Common symptoms include leg pain during walking (claudication), numbness, and coldness in the lower extremities. In severe cases, wounds on the feet or toes may fail to heal, leading to infections or gangrene.
The prevalence of PAD varies by age group. Among the general population, it affects 3-10%, while in individuals over 70, the prevalence rises to 10-20%. Without proper intervention, complications such as critical limb ischemia or even amputation may occur. These outcomes highlight the importance of recognizing symptoms early.
Age Group | Prevalence of PAD |
|---|---|
General Population | 3-10% |
Age > 70 | 10-20% |
Why timely treatment is crucial
Timely treatment of peripheral artery disease is essential to prevent severe complications. Early intervention can restore blood flow, alleviate symptoms, and improve quality of life. Delayed treatment increases the risk of irreversible damage, including limb loss. Advanced therapies, such as nitinol stents, offer effective solutions for managing this condition. These stents enhance blood flow and reduce the likelihood of complications, making them a vital tool in modern medicine.
Early diagnosis and treatment can significantly reduce the burden of peripheral arterial disease, ensuring better outcomes for patients worldwide.
Traditional Approaches to Arterial Disease Treatment
Common methods like angioplasty and bypass surgery
For decades, angioplasty and bypass surgery have been the cornerstone treatments for arterial diseases. Angioplasty, particularly balloon angioplasty, involves inserting a small balloon into the narrowed artery. Once inflated, the balloon compresses the plaque against the artery walls, restoring blood flow. This minimally invasive procedure is often used for patients with mild to moderate arterial blockages.
Bypass surgery, on the other hand, is a more invasive approach. Surgeons create a new pathway for blood flow by grafting a healthy blood vessel from another part of the body. This method is typically reserved for severe cases where angioplasty may not be effective.
Clinical trials have shown the effectiveness of these methods. For instance:
Coronary artery bypass surgery proved more effective than angioplasty for certain patient groups.
Among patients with diabetes, the five-year mortality rate was 12% for bypass surgery compared to 20% for angioplasty.
For patients older than 65, the mortality rate was 11% for bypass surgery versus 15% for angioplasty.
These findings highlight the importance of selecting the right treatment based on individual patient factors.
Limitations of traditional treatments
Despite their effectiveness, traditional treatments like angioplasty and bypass surgery have limitations. Balloon angioplasty, while minimally invasive, may not provide long-term results for all patients. Arteries can re-narrow over time, a condition known as restenosis. Additionally, bypass surgery carries significant risks due to its invasive nature, including infection, blood clots, and extended recovery periods.
Both methods may also fail to address the underlying causes of arterial disease, such as plaque buildup and vascular damage. These limitations underscore the need for more advanced and durable solutions.
The need for advanced solutions
The growing prevalence of arterial diseases highlights the need for innovative treatments. Significant demographic disparities exist in the incidence of lower extremity peripheral arterial disease (LEPAD). Women often experience higher rates of disability, while older adults face accelerated vascular deterioration. Regional disparities also persist, with low-income regions experiencing rising rates due to factors like high smoking prevalence and limited healthcare access.
Advanced solutions, such as nitinol stents, offer hope for addressing these challenges. Their unique properties, including flexibility and durability, make them a promising alternative to traditional methods like balloon angioplasty. By providing long-term results and reducing complications, these innovations can improve outcomes for patients worldwide.
How Nitinol Stents Work

Unique properties of nitinol (shape memory and superelasticity)
Nitinol, a nickel-titanium alloy, possesses two remarkable properties that make it ideal for use in stents: shape memory and superelasticity. These characteristics allow nitinol stents to adapt to the dynamic environment of the human body, particularly in arteries like the femoropopliteal artery and superficial femoral artery, which experience constant movement and stress.
Shape memory enables nitinol to return to its original shape after deformation when exposed to a specific temperature. For example, a nitinol wire bent in cold water retains its deformed shape but regains its original form when heated. This property ensures that nitinol stents can be compressed for insertion and then expand to their intended shape once deployed in the artery. Superelasticity, on the other hand, allows nitinol to undergo significant deformation and recover without permanent damage. This flexibility is crucial for stents placed in arteries that bend and stretch during everyday activities.
Property | Description |
|---|---|
Superelasticity | Nitinol exhibits superelasticity, allowing it to return to its original shape after deformation when above a critical temperature. |
Shape Memory | Nitinol can recover its original shape from a deformed state when heated above its transformation temperature. |
Experimental Setup | Demonstrations include bending nitinol wire in cold water, where it retains the bend, and then heating it to show recovery. |
These unique properties make nitinol stents highly effective in maintaining arterial patency, even in challenging vascular environments.
Deployment and placement of nitinol stents
The deployment of nitinol stents involves a minimally invasive procedure known as endovascular stenting. During this process, a catheter delivers the stent to the affected artery, such as the superficial femoral artery or femoropopliteal artery. The stent is compressed within the catheter to facilitate its passage through the vascular system. Once it reaches the target site, the stent expands to its pre-designed shape, thanks to the shape memory property of nitinol.
This expansion stabilizes the arterial walls and restores blood flow by keeping the artery open. The superelasticity of nitinol ensures that the stent can withstand the mechanical forces exerted by the artery's natural movements. Unlike balloon angioplasty, which relies on external pressure to widen the artery, nitinol stents provide a self-expanding solution that adapts to the artery's shape and size.
The placement of nitinol stents is particularly advantageous in areas prone to high stress and movement. For instance, the femoropopliteal artery experiences significant bending and twisting during walking. Nitinol stents maintain their structural integrity in such conditions, reducing the risk of complications like stent fractures or restenosis.
How nitinol stents improve blood flow
Nitinol stents significantly enhance blood flow in arteries affected by peripheral arterial disease. By expanding within the artery, these stents counteract the narrowing caused by plaque buildup. This results in improved blood flow to the limbs, alleviating symptoms such as claudication and coldness in the extremities.
Hemodynamic studies have demonstrated the effectiveness of nitinol stents in improving arterial function. For example, a prospective, randomized trial involving 76 patients compared the performance of BioMimics 3D nitinol stents to traditional stents. The results showed a primary patency rate of 72% for BioMimics 3D stents at two years, compared to 55% for the control group. Additionally, 87% of patients treated with BioMimics 3D stents experienced an improvement in Rutherford categories, indicating better symptom management and quality of life.
Evidence Type | Description |
|---|---|
Study Design | Prospective, randomized, multicenter controlled trial |
Patient Enrollment | 76 patients (50 BioMimics 3D, 26 Control) |
Primary Patency at 2 Years | 72% for BioMimics 3D vs. 55% for Control (P<0.05) |
Improvement in Rutherford Categories | 87% of BioMimics 3D patients improved at 24 months |
Stent Fractures | No fractures detected in BioMimics 3D stents |
Curvature Comparison | BioMimics 3D stents showed significantly greater curvature (P=0.02) |
Hemodynamic Effect | Evidence of secondary (swirling) flow and elevated wall shear stress in BioMimics 3D stents |
The ability of nitinol stents to maintain arterial patency and promote swirling blood flow reduces the risk of restenosis. This ensures long-term success in the treatment of peripheral artery disease, offering patients a durable and effective solution.
Advantages of Nitinol Stents for Arterial Diseases

Minimally invasive procedure
Nitinol stents offer a minimally invasive treatment option for peripheral arterial disease. Unlike traditional surgical methods, such as bypass surgery, the placement of nitinol stents involves a catheter-based procedure. This approach reduces the need for large incisions, leading to shorter recovery times and fewer complications. Patients undergoing this procedure often experience less pain and a quicker return to daily activities.
Clinical data highlights the effectiveness of this minimally invasive treatment. For example, procedural success rates for nitinol stent implantation reach 98.2%, with a technical success rate of 100%. Additionally, patients show significant improvements in walking capacity, with an average increase of 147 meters. The mean ankle-brachial index, a measure of blood flow, improves from 0.70 to 0.95. These outcomes demonstrate the reliability and efficiency of nitinol stents in restoring arterial function.
Metric | Value |
|---|---|
Technical success rate | 100% |
Procedural success rate | 98.2% |
Restenosis rate at 6 months | 8.5% |
Mean ankle-brachial index | Improved from 0.70 to 0.95 |
Improvement in walking capacity | Average of 147 m |
Rutherford index improvement | 72% |
Symptom deterioration | 0 patients |
Stent fracture cases | 1 case |
The minimally invasive nature of nitinol stents makes them an ideal choice for patients seeking effective treatment with reduced risks and faster recovery.
Long-term durability and flexibility
Nitinol stents are designed to withstand the challenging conditions of the vascular system. Their unique properties, including shape memory and superelasticity, allow them to adapt to the dynamic environment of arteries like the femoropopliteal artery and superficial femoral artery. These arteries experience constant movement due to activities such as walking, making flexibility a critical factor for stent performance.
Studies reveal the impressive durability of nitinol stents. For instance:
Nitinol stents in the femoropopliteal artery exhibit bending stiffness values ranging from 2 N/m (Tigris) to 98 N/m (Smart Control).
Axial tensile stiffness varies significantly, with Viabahn being the stiffest at 12,387 N/m and Misago being the most compliant at 32 N/m.
Patency rates for endovascular femoropopliteal artery stent-based repairs range from 43% to 90% at 12 months.
Additionally, nitinol stents endure approximately 420 million loading cycles over 10 years due to heartbeat-induced pulsations. Despite these challenges, their design minimizes the risk of fractures and ensures long-term performance. The geometry and material composition of nitinol stents play a crucial role in their fatigue resistance, making them a reliable solution for arterial treatments.
Enhanced blood flow and symptom relief
Nitinol stents significantly improve blood flow in arteries affected by peripheral arterial disease. By expanding within the artery, these stents counteract narrowing caused by plaque buildup. This results in improved blood flow to the limbs, alleviating symptoms such as claudication and coldness in the extremities.
The VIBRANT Trial provides compelling evidence of the effectiveness of nitinol stents. This clinical trial compared bare-nitinol stents to stent grafts in treating long lesions in the superficial femoral artery. The results demonstrated enhanced blood flow and symptom relief, with primary patency maintained over three years. Patients also reported improved quality of life through standardized questionnaires, underscoring the benefits of nitinol stents in managing peripheral arterial disease.
By restoring arterial patency and reducing symptoms, nitinol stents offer a durable and effective solution for patients. Their ability to maintain improved blood flow ensures better long-term outcomes and a higher quality of life.
Improved quality of life for patients
Nitinol stents have revolutionized the treatment of arterial diseases, offering patients a significant improvement in their quality of life. These medical devices address the root cause of restricted blood flow, enabling individuals to regain mobility and independence. By alleviating symptoms such as pain and numbness, nitinol stents allow patients to engage in daily activities with greater ease and comfort.
One of the most notable benefits of nitinol stents is their ability to restore physical functionality. Patients with peripheral arterial disease often experience difficulty walking due to claudication. This condition limits their ability to perform even basic tasks. After receiving nitinol stents, many patients report a dramatic increase in their walking distance and stamina. Clinical studies have shown that individuals treated with these stents can walk farther without pain, enhancing their overall physical well-being.
The psychological impact of improved mobility cannot be overlooked. Chronic pain and limited movement often lead to feelings of frustration and depression. Nitinol stents help alleviate these emotional burdens by providing a reliable solution to arterial blockages. Patients frequently describe a renewed sense of hope and confidence after treatment. This positive shift in mental health contributes to a more fulfilling and active lifestyle.
Another critical aspect of improved quality of life is the reduction in medical complications. Nitinol stents minimize the risk of severe outcomes such as critical limb ischemia and amputation. By maintaining arterial patency, these devices ensure consistent blood flow to the limbs. This reduces the likelihood of infections and promotes faster healing of wounds. Patients benefit from fewer hospital visits and a lower need for additional interventions, which translates to less financial and emotional strain.
The durability and flexibility of nitinol stents also play a crucial role in enhancing patient outcomes. These stents adapt to the natural movements of the body, ensuring long-term functionality. Unlike traditional treatments, which may require frequent follow-ups or revisions, nitinol stents provide a lasting solution. This reliability allows patients to focus on their recovery and enjoy a higher quality of life without constant medical concerns.
In addition to physical and emotional benefits, nitinol stents contribute to social and professional well-being. Improved mobility enables patients to participate in social activities and maintain their professional responsibilities. This fosters a sense of normalcy and inclusion, which is essential for overall happiness and satisfaction. The ability to engage with family, friends, and colleagues enhances the social fabric of a patient's life, creating a positive ripple effect on their community.
The transformative impact of nitinol stents extends beyond individual patients. Families and caregivers also experience relief as their loved ones regain independence. The reduced need for caregiving allows families to focus on strengthening their relationships rather than managing medical challenges. This holistic improvement underscores the far-reaching benefits of nitinol stents in treating arterial diseases.
Patient Eligibility and Expected Outcomes
Who can benefit from nitinol stents?
Nitinol stents are suitable for individuals with arterial diseases, particularly those affecting the femoropopliteal artery and superficial femoral artery. Patients with peripheral arterial disease (PAD) who experience symptoms like claudication or critical limb ischemia often benefit from these stents. They are especially effective for individuals with arteries prone to movement, as nitinol's flexibility ensures durability in dynamic vascular environments.
Candidates for nitinol stents typically include those who have not responded well to traditional treatments like angioplasty or bypass surgery. Patients with long arterial lesions or recurring blockages also find these stents advantageous. However, eligibility depends on factors such as the severity of the arterial narrowing, overall health, and the presence of comorbidities like diabetes or hypertension. Physicians assess these factors to determine the best course of action.
Factors influencing treatment decisions
Several factors influence the decision to use nitinol stents. The location and length of the arterial blockage play a significant role. For instance, the femoropopliteal artery and superficial femoral artery are common sites for stent placement due to their susceptibility to stress and movement. The patient's age, lifestyle, and medical history also impact the choice of treatment. Younger, active individuals may benefit more from nitinol stents due to their flexibility and long-term durability.
The type of arterial disease also matters. Nitinol stents are often preferred for PAD cases involving complex or calcified lesions. Additionally, the patient's ability to undergo a minimally invasive procedure is considered. Those with conditions that increase surgical risks may find nitinol stents a safer alternative to bypass surgery.
Recovery process and long-term results
The recovery process after nitinol stent implantation is typically smooth due to the minimally invasive nature of the procedure. Most patients resume normal activities within a few days. Regular follow-ups ensure the stent remains effective and complications are avoided. Patients often experience immediate symptom relief, including reduced pain and improved mobility.
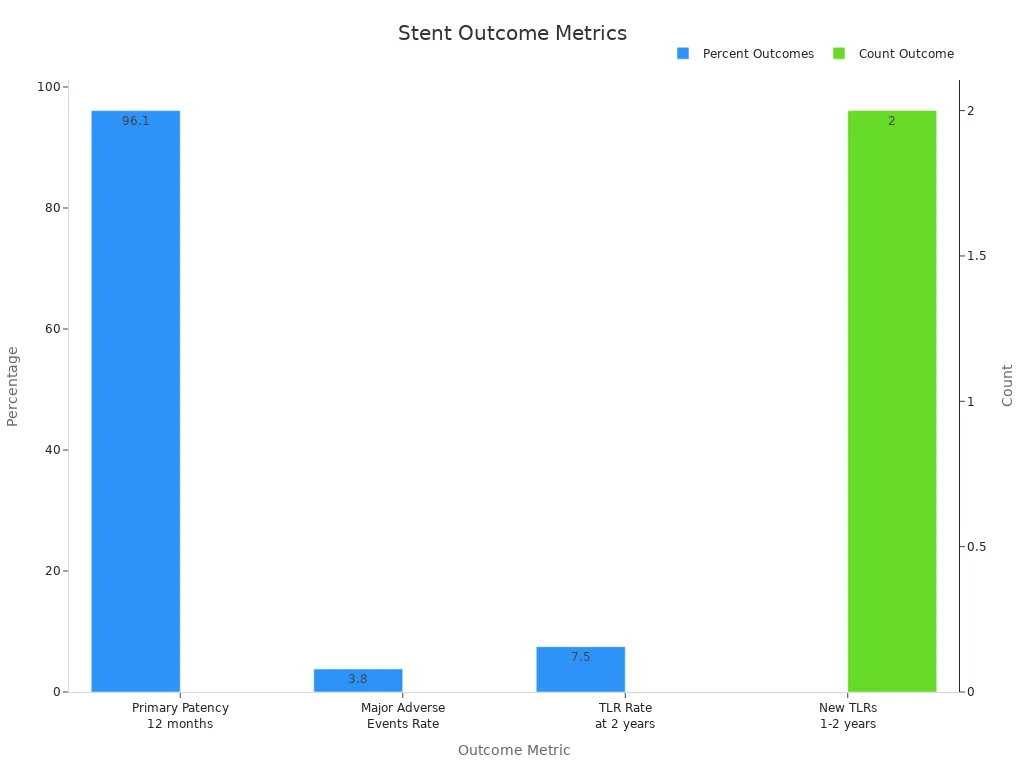
Long-term outcomes for nitinol stents are promising. Studies show a primary patency rate of 96.1% at 12 months, with a low major adverse event rate of 3.8%. Target lesion revascularization rates remain low, with only 7.5% of patients requiring additional procedures within two years. These results highlight the durability and effectiveness of nitinol stents in maintaining arterial patency.
The ability of nitinol stents to adapt to the natural movements of the femoropopliteal artery and superficial femoral artery ensures long-term success. Patients report significant improvements in quality of life, including increased walking distance and reduced symptoms. These outcomes make nitinol stents a reliable solution for managing arterial diseases.
Nitinol stents have transformed arterial disease treatment by offering minimally invasive solutions that improve blood flow and reduce complications. Their unique properties, including shape memory and superelasticity, ensure durability and flexibility in dynamic vascular environments. Patients experience enhanced mobility, reduced symptoms, and a better quality of life after receiving these stents.
The global market for nitinol stents reflects their growing importance. Valued at $1.5 billion in 2023, it is projected to reach $3.2 billion by 2032, driven by advancements in stent technology and rising demand for minimally invasive procedures. Nitinol's biocompatibility and self-expansion capabilities make it ideal for treating vascular diseases. As healthcare infrastructure improves in regions like Asia Pacific, the adoption of nitinol stents is expected to rise, further enhancing patient outcomes.
Future advancements in nitinol stent technology promise even greater benefits. Innovations in design and material composition will likely improve performance and expand applications. These developments will continue to address the growing prevalence of vascular diseases, ensuring better treatment options for patients worldwide.
FAQ
What are nitinol stents made of?
Nitinol stents consist of a nickel-titanium alloy. This material provides unique properties like shape memory and superelasticity, which allow the stents to adapt to the dynamic movements of arteries while maintaining their structural integrity.
How do nitinol stents differ from traditional stents?
Nitinol stents offer flexibility and durability due to their superelasticity. Unlike traditional stents, they self-expand and adapt to arterial movements, making them ideal for areas prone to stress, such as the femoropopliteal artery.
Are nitinol stents safe for all patients?
Nitinol stents are generally safe for most patients with arterial diseases. However, eligibility depends on factors like the severity of the blockage, overall health, and the presence of conditions like diabetes or hypertension.
How long do nitinol stents last?
Nitinol stents are designed for long-term durability. Studies show high patency rates and minimal complications over several years, making them a reliable solution for arterial disease treatment.
What is the recovery process after stent placement?
Recovery after nitinol stent placement is quick due to the minimally invasive procedure. Most patients resume normal activities within days and experience immediate symptom relief, including improved mobility and reduced pain.
See Also
Nitinol Tubing's Impact on Modern Medical Innovations
Investigating Nitinol Tubing Uses in Medical Equipment
The Manufacturing Process of Nitinol Tubing for Medicine

