How Laser-Cut Nitinol Tubing Shapes Modern Stent Retrievers

Laser-cut nitinol tubing for stent retrievers forms the backbone of many advanced medical devices used in neurovascular applications. Precision in manufacturing directly affects device performance and patient safety. Structural analysis shows that even small changes in stent design can improve first-pass success during mechanical thrombectomy. Many medical applications depend on nitinol for its flexibility and strength. In clinical studies, high technical and clinical success rates link to precise control in medical procedures. Tight tolerances in manufacturing, such as those achieved with PTFE glass mandrels, help reduce risks and improve consistency across medical applications.
Key Takeaways
Laser-cut nitinol tubing allows precise and flexible stent designs that improve clot removal in stroke treatment.
Open-cell stent designs offer better flexibility and support, leading to higher success rates in clinical use.
Femtosecond laser cutting creates clean, accurate stents without damaging the material, preserving its strength and shape memory.
Heat treatment and electropolishing enhance stent durability and safety by improving surface quality and mechanical properties.
Clinical studies show laser-cut nitinol stent retrievers increase patient recovery rates and reduce complications during thrombectomy.
Laser-Cut Nitinol Tubing for Stent Retrievers
Mesh Structure Creation
Laser-cut nitinol tubing for stent retrievers allows engineers to create very precise mesh structures. They use advanced lasers to cut patterns into small-diameter nitinol tube. This process shapes the stent so it can expand and grip blood clots during procedures. Laser cutting gives much more control than older methods like knitting or braiding. With laser technology, each cut can be measured and repeated exactly, which is important for stent applications that demand high accuracy.
Researchers have shown that using photolithography-based laser cutting, followed by chemical etching and heat treatment, improves both the surface quality and the mechanical properties of nitinol stents. Bench tests and computer models confirm that these stents have better elasticity and can adapt to the shape of blood vessels. Another study found that laser cutting can create micro-patterned surfaces on stents, which helps them remove clots more efficiently. Even though laser cutting can leave tiny burrs, special treatments like electropolishing remove these and keep the mesh smooth.
The effectiveness of laser-cut nitinol tubing for stent retrievers depends on precise measurements. For example, a laser frequency of 8 Hz and a power of 1 kW give the best results for cell health and stent strength. A spot size of 0.6 mm works well for mechanical strength, while thermal annealing at 500°C for 30 minutes improves both biocompatibility and durability. Devices made with these settings show strong performance in delivery and retrieval tests.
Laser-cut nitinol tubing for stent retrievers offers unmatched design flexibility. Engineers can change the mesh pattern to fit different medical needs, making it easier to treat a wide range of patients.
Open-Cell and Closed-Cell Designs
Laser-cut nitinol tubing for stent retrievers supports both open-cell and closed-cell designs. Open-cell stents have gaps between the struts, which makes them more flexible. This flexibility helps the stent move through winding blood vessels and grip clots better. Closed-cell stents have connected struts, forming a cage-like structure. These stents are less flexible but may provide more support in certain cases.
Comparative studies show that open-cell stents often perform better in clinical use. For example, open-cell stents have higher patency rates at both 6 and 12 months after placement. They also show better flexibility, radial strength, and less risk of shortening or moving out of place. Closed-cell stents sometimes face problems with migration during breathing or vessel movement.
Stent Type | 6-month Primary Patency | 12-month Primary Patency | Mean Patency (months) | Notes on Performance and Properties |
|---|---|---|---|---|
Open-cell | 64.8% | 28.8% | 10.9 ± 0.80 | Higher flexibility, radial strength, and expansibility; less shortening and migration |
Closed-cell | 38.7% | 16.0% | 8.5 ± 10.87 | Issues with shortening and migration during respiration |
Finite element analysis shows that open-cell stent retrievers provide better support and more complete contact with the clot.
Open-cell designs help improve the success of clot removal, especially for tough clots.
Biomechanical studies confirm that open-cell stents are more flexible and effective than closed-cell designs.
Computer models show that open-cell stents optimize how the device interacts with both the clot and the vessel wall.
High-quality laser cut stents made from nitinol give doctors more options. They can choose the best design for each patient, improving the chances of a successful procedure. The flexibility and strength of nitinol, combined with the accuracy of laser cutting, make these stents a top choice for modern stent retriever devices.
Laser Cutting Process
Femtosecond Laser Technology
Femtosecond laser stent cutting uses ultrashort pulses to shape nitinol tubing with high precision. Each pulse lasts less than 300 femtoseconds. This cold ablation process removes material without heating the stent. Engineers prefer femtosecond laser stent cutting because it avoids melting, microcracks, and deformation. The process keeps the stent’s shape memory and superelasticity intact. Optical microscope images show clean edges and smooth surfaces after femtosecond laser stent cutting. This method achieves a cutting accuracy of ±0.05 mm, which meets strict medical standards. The process also supports intricate mesh designs for stents used in complex blood vessels.
Specification | Description |
|---|---|
Pulse Duration | < 300 femtoseconds |
Cutting Accuracy | ±0.05 mm |
Thermal Effects | No heat-affected zone |
Edge Quality | Clean-cut edges |
Application Suitability | Ideal for medical stent manufacturing |
Process Stability | Enhanced by AI and real-time monitoring |
Laser cutting nitinol with femtosecond lasers produces smooth surfaces and reduces the need for extra finishing steps. This technology helps maintain the original properties of nitinol, which is important for stent performance.
Heat Treatment and Electropolishing
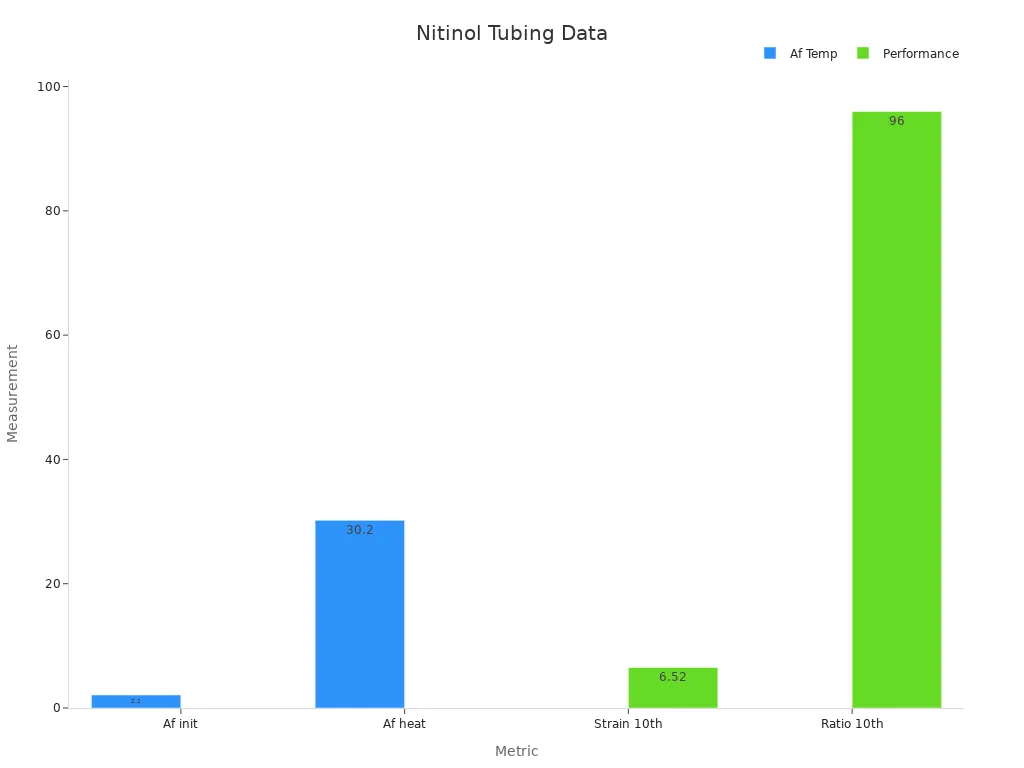
After laser cutting, heat treatment and electropolishing improve the stent’s durability and surface quality. Heat treatment raises the Af transformation temperature of nitinol from 2.1°C to 30.2°C. This change increases the stent’s ability to recover its shape and improves its mechanical strength. The recovery ratio stays above 90% even after many cycles, showing strong durability.
Metric | Value |
|---|---|
Af temperature (initial) | 2.1°C |
Af temperature (after heat treatment) | 30.2°C |
Recovery ratio (2nd cycle) | > 90% |
Stable recoverable strain (10th cycle) | 6.52% |
Recovery ratio (10th cycle) | 96% |
Electropolishing smooths the stent’s surface and removes tiny burrs left from laser cutting. Dry electropolishing improves surface roughness by a factor of 10, making the stent safer and more resistant to corrosion. This step also helps the stent move smoothly through blood vessels.
Burr Control and Inert Gas Use
Burr control is important for making safe and reliable stents. During laser cutting, engineers use inert gases like argon to prevent oxidation and material degradation. This moisture-free environment keeps the stent’s surface clean and reduces defects. Studies show that using oxygen assist gas can lower surface roughness to about 18 µm, while inert gas keeps it around 22 µm. Multi-pass cutting also helps reduce dross and burrs, leading to cleaner stent edges.
Metric | Oxygen Assist Gas | Air Assist Gas | Inert Gas Assist | Additional Technique |
|---|---|---|---|---|
Surface Roughness (µm) | ~18 | ~29 | ~22 | Multi-pass cutting reduces dross formation |
Laser cutting technology, combined with careful burr control and inert gas use, ensures that each stent meets high standards for safety and performance.
Stent Retriever Thrombectomy

Thrombectomy Procedure Overview
Doctors use stent retriever thrombectomy to treat patients with stroke. This procedure removes a clot that blocks blood flow in the brain. When a person has an acute ischemic stroke, a clot forms in a blood vessel and stops oxygen from reaching brain tissue. Quick removal of the clot can save brain cells and improve recovery.
During the thrombectomy procedure, a doctor inserts a thin tube into an artery, usually in the groin. The tube travels through the blood vessels to reach the blocked area in the brain. The doctor then deploys a stent retriever, which expands inside the vessel and traps the clot. The stent grips the clot firmly, allowing the doctor to pull both the stent and the clot out together. This restores blood flow and reduces the risk of long-term damage.
Clinical studies show that stent retrievers made from laser-cut nitinol tubing improve outcomes for stroke patients.
These devices increase the chance of a good recovery by 74% compared to medicine alone.
They reduce death and disability by more than half.
The superelasticity and shape memory of nitinol help the stent move through winding vessels and expand inside the clot.
Special design features, such as radiopaque markers, help doctors see the stent during the procedure and position it correctly.
Device Performance in Clot Removal
Stent retrievers with laser-cut nitinol tubing show strong performance in clot removal. The precise mesh structure grips the clot and keeps it from breaking apart. The stent’s design helps it stay in contact with the vessel wall, which improves clot capture and lowers the risk of pieces breaking off.
A preclinical study compared a laser-cut nitinol stent retriever with a well-known device. Both devices achieved high recanalization rates, showing that laser-cut nitinol designs work as well as established thrombectomy devices. The laser-cut stent caused less damage to blood vessels, thanks to its balanced radial force and wide mesh area. This reduces the risk of injury during the thrombectomy procedure.
Performance metrics highlight the advantages of these stents:
Parameter | Solitaire FR (Commercial) | Stent D (Laser-cut Nitinol) |
|---|---|---|
Thrombus Retrieval Rate (%) | 96.16% | 95.51% |
Radial Force (N) | 3.77 ± 0.01 | 4.10 ± 0.07 |
Flexibility (N) | 0.38 ± 0.11 | 0.59 ± 0.05 |
Deployment Force (N) | 0.37 ± 0.02 | 0.32 ± 0.02 |
Recapture Force (N) | 0.38 ± 0.01 | 0.35 ± 0.01 |
Doctors see high rates of complete recanalization and immediate flow restoration with these stents. Imaging shows that the clot stays straight and does not compress or stretch during retrieval. This means the stent holds the clot firmly, making removal more effective and reducing trauma to the vessel. Stent retriever thrombectomy with laser-cut nitinol devices gives patients with stroke a better chance at recovery and a lower risk of complications.
Clinical Impact
Patient Outcomes
Laser-cut nitinol stent retrievers have changed the way doctors treat stroke. These medical devices help restore blood flow by removing the clot that blocks a vessel in the brain. Doctors see high recanalization success rates, reaching up to 94.8% in patients treated with the pREset stent retriever. Patients who achieve successful recanalization often show strong clinical improvement after thrombectomy. No patients with incomplete recanalization reach a favorable outcome at discharge or follow-up.
High recanalization success rate (TICI 2b/3) up to 94.8%
Significant link between successful recanalization and lower mortality within 90 days
Favorable neurological outcome (mRS 0–2) at mid-term follow-up is about 41.9%
Low complication rates support the safety of these devices
Clinical results match or exceed those of other second-generation stent retrievers
The following table shows long-term patient outcomes after treatment with laser-cut nitinol stent retrievers:
Outcome Measure | Statistic / Result | Notes / Significance |
|---|---|---|
Mortality within 90 days (TICI 2b/3) | 8.6% | Lower than with unsuccessful recanalization |
Mortality within 90 days (TICI 0–2a) | 62.5% | High mortality with unsuccessful recanalization |
Favorable outcome (mRS 0–2) at discharge (TICI 2b/3) | Significantly higher proportion | Better functional outcome after successful recanalization |
Favorable outcome (mRS 0–2) at mid-term follow-up | 41.9% | Comparable to other registries |
Favorable outcome (mRS 0–2) at discharge (TICI 0–2a) | 0% | No favorable outcome after unsuccessful recanalization |
Favorable outcome (mRS 0–1) at follow-up (TICI 0–2a) | 0% | No very good outcome after unsuccessful recanalization |
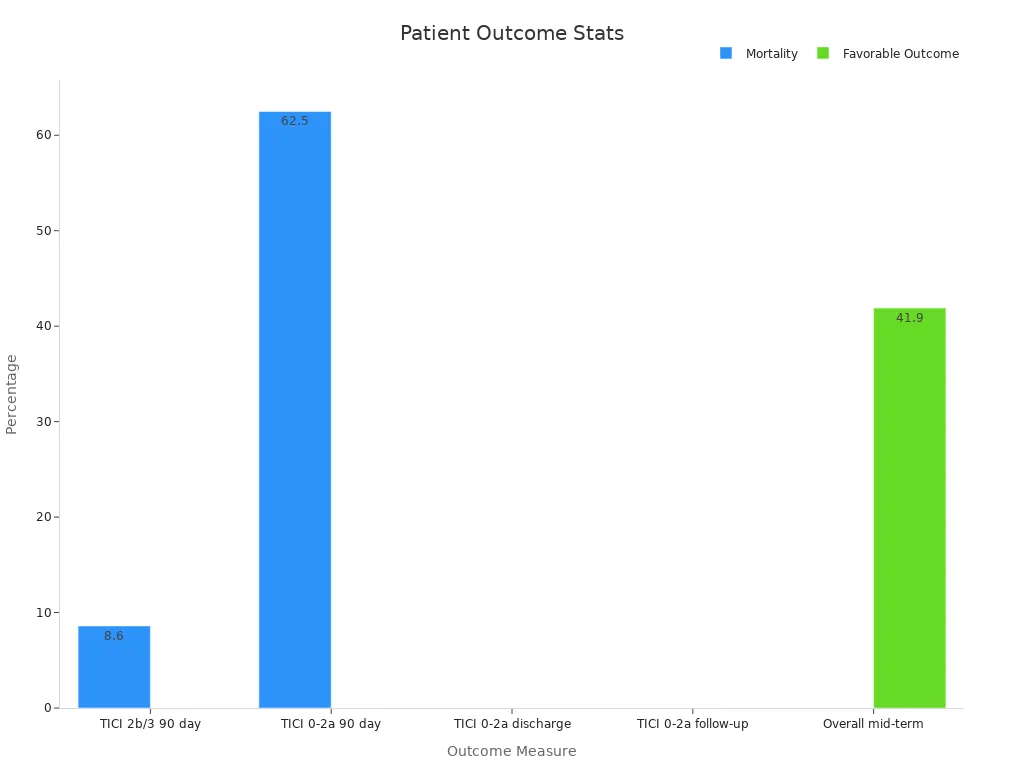
These results highlight the importance of successful clot removal in stroke treatment. Laser-cut nitinol stent retrievers play a key role in improving survival and recovery.
Safety and Reliability
Doctors trust laser-cut nitinol stent retrievers for their safety and reliability in medical device applications. Nitinol’s superelasticity and shape memory allow the stent to expand inside the vessel and grip the clot without causing damage. Surface treatments like electropolishing make the device more biocompatible and resistant to corrosion. Clinical data show that nitinol-based neurovascular devices help patients recover about 20% faster than those treated with traditional materials. These devices also reduce the risk of complications during and after the procedure.
Nitinol stents perform well in treating wide-necked intracranial aneurysms and other neurovascular applications. The material’s phase transformation properties help the stent recover its shape after deformation, ensuring consistent performance. Studies report minimal tissue reactions and strong durability, which support long-term safety.
A major clinical trial, PROST, compared the pRESET laser-cut nitinol stent retriever to the established Solitaire device in 340 patients with large vessel occlusion stroke. The trial found that pRESET was just as safe and effective as Solitaire for thrombectomy. Both devices showed similar rates of functional independence at 90 days and low complication rates.
Aspect | Details |
|---|---|
Trial Name | PROST (pRESET for Occlusive Stroke Treatment) |
Devices Compared | pRESET (laser-cut nitinol stent retriever) vs Solitaire |
Patient Population | 340 patients with large vessel occlusion stroke |
Primary Outcome | Functional independence at 90 days (mRS) |
Key Findings | pRESET noninferior to Solitaire (54.9% vs 57.5%) |
Conclusion | pRESET is a safe and effective alternative for thrombectomy |
Laser-cut nitinol stent retrievers continue to set new standards for safety, reliability, and performance in medical applications. Their success in stroke and thrombectomy procedures points to even greater innovation in future neurovascular devices.
Laser-cut nitinol tubing has transformed medical stent retriever technology. Precision in manufacturing gives medical devices the flexibility and strength needed for safe navigation in delicate brain vessels. Medical teams now see better patient outcomes because these stents expand and compress as needed, reducing complications. Medical device makers continue to improve tubing with new designs, digital features, and rapid prototyping. Future neurovascular devices will use these advances to deliver safer, more reliable medical care.
FAQ
What is nitinol and why do stent retrievers use it?
Nitinol is a metal alloy made from nickel and titanium. Stent retrievers use nitinol because it bends easily and returns to its original shape. This helps the device move through blood vessels and grip clots.
How does laser cutting improve stent retriever design?
Laser cutting creates precise patterns in nitinol tubing. This process allows engineers to design stents with exact shapes and sizes. The result is a device that fits better in blood vessels and removes clots more effectively.
Are laser-cut nitinol stent retrievers safe for patients?
Doctors trust laser-cut nitinol stent retrievers because they show high safety in clinical studies. The smooth surface and strong structure lower the risk of vessel injury. Most patients recover well after treatment with these devices.
What is the difference between open-cell and closed-cell stent designs?
Open-cell stents have gaps between the struts, making them flexible. Closed-cell stents have connected struts, giving more support. Doctors choose the design based on the patient’s needs and the shape of the blood vessel.
Can doctors see the stent retriever during the procedure?
Yes! Stent retrievers often have radiopaque markers. These markers show up on X-ray images, so doctors can watch the device move and place it correctly inside the blood vessel.
See Also
Transforming Medical Devices Through Innovative Nitinol Tubing
The Process Behind Manufacturing Nitinol Tubing For Medicine
Nitinol Tubing’s Impact On Progressing Medical Technology
A Deep Dive Into Nitinol Tubing Uses In Healthcare
The Importance Of Nitinol Tubing In Minimally Invasive Surgery

