What High-Radial-Force Nitinol Tubing Means for Thrombectomy Stents

High-radial-force nitinol tubing for thrombectomy stents uses a special alloy that provides both flexibility and strength. In thrombectomy, the stent must push outward to press against a blood clot and restore blood flow, which is vital for patients with acute ischemic stroke. The PROST randomized clinical trial compared stent retrievers and showed that radial force can improve clot removal and keep vessels open. Another study in a swine model revealed that while radial force can cause some vessel wall changes, the relationship between force and vessel injury is complex. Designers of thrombectomy devices aim to find the right balance, so the stent removes clots effectively but does not harm the vessel.
Key Takeaways
High-radial-force nitinol tubing gives thrombectomy stents the strength and flexibility needed to grip and remove blood clots effectively.
Proper radial force helps stents press against clots and vessel walls, improving clot removal and restoring blood flow in stroke patients.
Designers must balance radial force to avoid vessel injury while ensuring strong clot engagement and long-term vessel openness.
Clinical studies show nitinol stents achieve high recanalization rates and better vessel patency compared to other treatments.
Surface treatments like drug-eluting and ultra-hydrophilic coatings improve stent safety by reducing cell overgrowth and promoting healing.
High-Radial-Force Nitinol Tubing for Thrombectomy Stents

Nitinol Properties
Nitinol stands out as a material for medical devices because of its unique combination of superelasticity, shape memory, and biocompatibility. These features make high-radial-force nitinol tubing for thrombectomy stents especially valuable. Superelasticity allows nitinol to stretch and return to its original shape, even after significant deformation. Shape memory means the stent can expand to its intended size once deployed inside the vessel. Biocompatibility ensures that the body tolerates the stent, reducing the risk of inflammation or rejection.
Note: Nitinol’s superelastic behavior helps stents adapt to the natural curves and movements of blood vessels, which is critical during thrombectomy procedures.
Clinical studies highlight the benefits of nitinol in stent performance:
The pRESET nitinol stent retriever achieves successful recanalization rates between 77% and 100%, with 86% to 96% in distal vessel blockages.
Patients treated with self-expanding stents made from nitinol show higher primary patency rates at 3, 6, and 12 months (85%, 63%, and 49%) compared to balloon angioplasty alone (32%, 24%, and 14%).
Median cumulative patency for nitinol stents reaches 260 days, while balloon angioplasty averages only 60 days.
These results demonstrate that high-radial-force nitinol tubing for thrombectomy stents supports both effective clot removal and long-term vessel openness.
Radial Force Explained
Radial force describes the outward pressure a stent applies against the vessel wall. In thrombectomy, this force plays a key role in pressing the stent against the clot, securing it for removal, and maintaining blood flow. High-radial-force nitinol tubing for thrombectomy stents delivers the strength needed to engage and compress clots without losing flexibility.
The design and construction of thrombectomy devices influence their radial force and clinical performance. The table below compares several leading stent retrievers:
Device | Construction Type | Radial Force Characteristics | Mechanical Test Findings | Clinical Recanalization Rate (TICI 2b/3) | Notes on Performance and Design |
|---|---|---|---|---|---|
EmboTrap | Two-layered laser-cut nitinol | Inner high radial force, outer lower radial force | Shows elongation in acute curves; fewer distal emboli in vitro compared to Solitaire | 84.6% (single center series) | Designed to optimize clot capture and reduce embolization; superior recanalization rates reported |
Solitaire | Laser-cut nitinol sheet | Closed cell, parametric overlapping design | Consistent wall apposition in tortuous vessels | ~71.1% (RCT data) | First dedicated stentriever; good clot integration; variable radial force depending on vessel diameter |
Trevo | Laser-cut tubular nitinol | Closed cell, tubular stent | Some loss of vessel wall contact in acute curves | 78.3% (early human data) | Braided platinum/tungsten wires for visualization; hydrophilic coating to reduce friction |
Mechanical tests show that high-radial-force nitinol tubing for thrombectomy stents, such as EmboTrap, provides strong radial force for clot engagement and maintains vessel patency. Clinical recanalization rates for these devices often exceed those of earlier designs.
A direct comparison between the Tonbridge and Solitaire FR stents further illustrates the impact of radial force:
Parameter | Tonbridge Stent | Solitaire FR Stent |
|---|---|---|
Radial Force | Slightly higher (in vitro test) | Slightly lower (in vitro test) |
Clot Engagement | Tighter clot engagement | Less tight engagement |
Recanalization Rate (Animal Study) | 100% | 88.9% |
Vessel Wall Injury Complications | No significant increase | No significant increase |
The Tonbridge stent, with its slightly higher radial force, achieves tighter clot engagement and a 100% recanalization rate in animal studies, compared to 88.9% for Solitaire FR. Both devices show no significant increase in vessel wall injury complications.
However, higher radial force can also increase the risk of vessel wall injury. Studies using high-resolution imaging reveal that stentrievers with greater radial force cause more arterial wall enhancement, a marker of endothelial damage, than aspiration catheters. Larger stents, which apply more force, achieve higher first-pass reperfusion rates but may also lead to more vessel wall changes, such as thickening and loss of elasticity.
High-radial-force nitinol tubing for thrombectomy stents must balance the need for strong clot engagement with the goal of minimizing vessel injury. Device design, number of passes, and stent size all influence this balance. Thrombectomy devices that use nitinol’s unique properties can optimize both safety and effectiveness for patients.
Thrombectomy Stent Requirements
Clot Engagement
A thrombectomy stent retriever must grip and remove blood clots efficiently to restore blood flow in patients with stroke. The device needs enough radial force to compress and secure the thrombus, even when the clot has a tough or mixed composition. Clinical trials, such as REVASCAT and MR-CLEAN, have shown that thrombectomy stent retrievers achieve recanalization rates above 70% in acute ischemic stroke patients. The following table summarizes key results:
Study/Measure | Numerical Result(s) | Description/Context |
|---|---|---|
REVASCAT trial | 70.5% recanalization rate (thrombectomy group) | Demonstrates effectiveness of stent retriever thrombectomy in acute ischemic stroke patients. |
MR-CLEAN trial | 75.4% recanalization rate (thrombectomy group) | Confirms high recanalization success with thrombectomy. |
90-day mRS score (0–2) | 43.7% (treatment) vs. 28.2% (control), OR=2.1 | Indicates better clinical outcomes post-thrombectomy. |
These results highlight the importance of strong clot engagement for successful outcomes.
Vessel Patency
Maintaining vessel patency after clot removal is essential for long-term recovery. Thrombectomy stent retrievers must keep the vessel open without causing damage. Registry data show that higher patency rates lead to better clinical success and fewer complications. The chart below illustrates outcome measures for vessel patency:
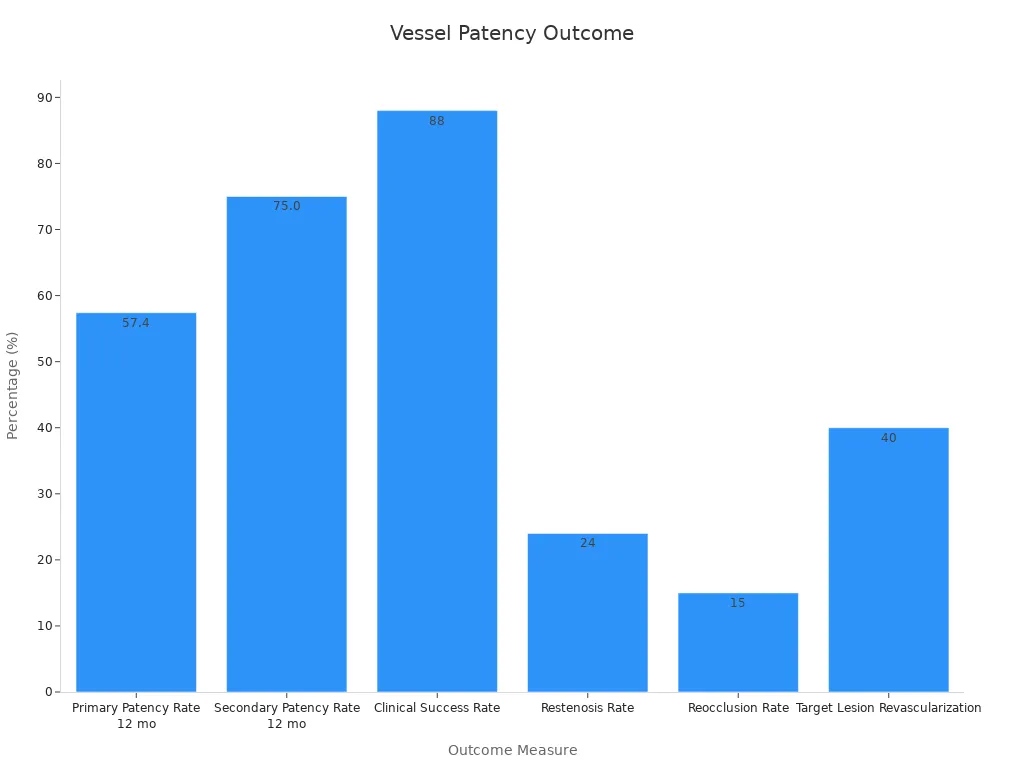
Primary patency at 12 months reaches 57.4%, while secondary patency is 75%. Clinical success rates approach 88%, showing the value of vessel patency in stroke treatment.
Safety Concerns
Thrombectomy devices must balance strong radial force with patient safety. Excessive radial force can injure vessel walls or cause perforation. Regulatory guidance stresses the need to measure and control radial force across different stent sizes. Studies confirm that wall thickness and stent flaring can increase stress on vessel tissue, raising the risk of injury. Careful design and testing help minimize these risks, ensuring that thrombectomy stent retrievers provide effective treatment for stroke without unnecessary complications.
Stent Outcomes
Clot Removal Efficiency
Clot removal efficiency remains a critical factor in the success of thrombectomy procedures for patients with stroke. Researchers have compared different stent designs using both laboratory models and clinical trials. In an in vitro study, scientists used a cerebrovascular phantom and artificial clots to test several stent retrievers. The optimized Stent D showed strong mechanical properties and removed clots more effectively than earlier designs. This improvement can help reduce procedure time and improve outcomes for acute ischemic stroke.
A systematic review and meta-analysis found that newer generation stent retrievers achieve higher recanalization rates and better patient outcomes than older devices. Randomized controlled trials, such as SWIFT and TREVO 2, confirmed that advanced retrievable stent designs outperform first-generation devices in clot removal. The ISAR-TEST 4 trial also demonstrated that new-generation stents with improved materials and coatings provide better long-term results, including lower rates of late stent thrombosis.
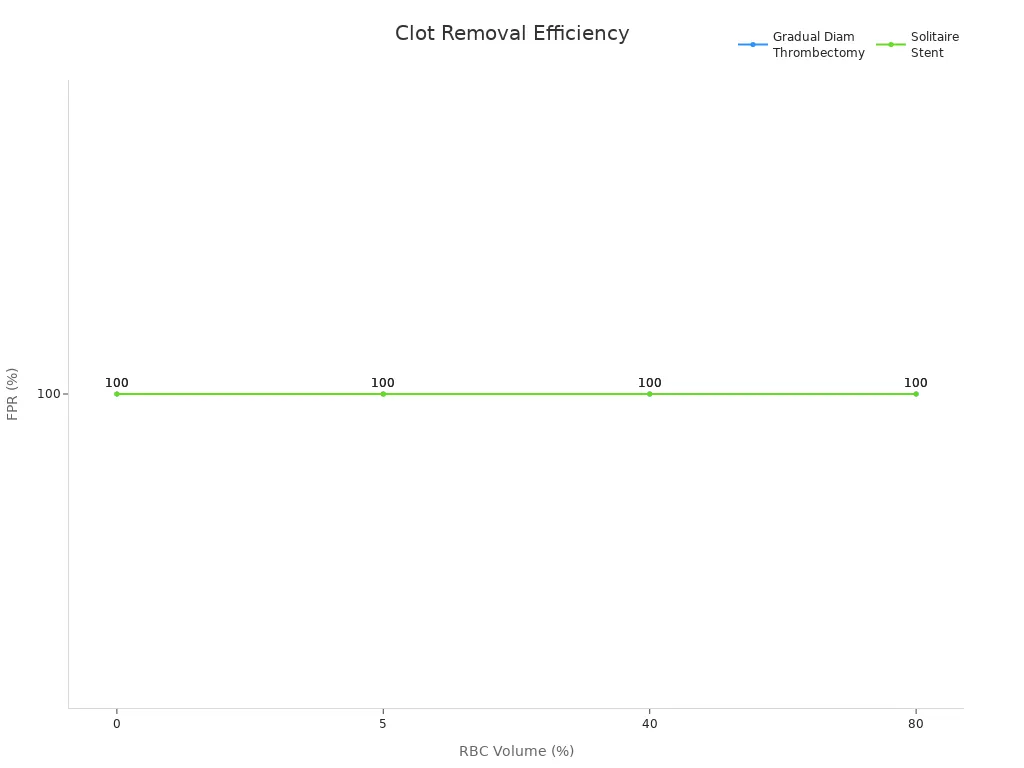
Statistical indicators further support these findings. The first-pass recanalization rate (FPR) measures how often a stent removes a clot on the first attempt. Both gradual diameter thrombectomy stents and Solitaire stents achieved a 100% FPR across clots with different red blood cell volumes. The table below summarizes these results:
Stent Type | RBC Volume (%) | First-Pass Recanalization Success Rate (%) | Thrombus Displacement Severity |
|---|---|---|---|
Gradual Diameter Thrombectomy | 0 | 100 | Severe |
Gradual Diameter Thrombectomy | 5 | 100 | Moderate |
Gradual Diameter Thrombectomy | 40 | 100 | Mild |
Gradual Diameter Thrombectomy | 80 | 100 | Mild |
Solitaire Stent | 0 | 100 | Severe |
Solitaire Stent | 5 | 100 | Moderate |
Solitaire Stent | 40 | 100 | Mild |
Solitaire Stent | 80 | 100 | Mild |
Vessel Wall Safety
Vessel wall safety is just as important as clot removal efficiency. The thrombectomy stent retriever must support the vessel without causing damage. Studies show that stents with moderate radial force perform better clinically, while excessive radial force can increase stress on the vessel wall and reduce flexibility. In vitro tests revealed that high radial force does not always guarantee ideal wall contact, and sometimes leads to suboptimal vessel wall impact.
Animal studies found that increasing stent radial force leads to thicker vessel walls and more neointimal hyperplasia, which can signal vessel injury. A numerical model identified an optimal deployment stress of 480 kPa, which maximizes vessel diameter while minimizing wall stress. This suggests that there is a threshold for radial force, beyond which vessel damage increases.
Clinical data also help quantify vessel wall safety. For example, the Tigertriever device showed a symptomatic intracranial hemorrhage (ICH) rate of 4% in a multi-center study, while the Penumbra 3D Revascularization Device had a 3.1% rate. These low rates of ICH, combined with high recanalization rates, suggest that current stent designs maintain an acceptable safety profile for vessel walls during stroke treatment.
Device / Study Cohort | Successful Recanalization Rate | First Pass Recanalization Rate | Symptomatic Intracranial Hemorrhage (ICH) Rate |
|---|---|---|---|
Tigertriever (61 patients) | 75.4% | 37.7% | N/A |
Tigertriever (repeat inflation-deflation subset) | 82.6% | 47.8% | N/A |
Multi-center Tigertriever experience | 74% | 36% | 4% |
Penumbra 3D Revascularization Device | 87.2% (TICI 2b/3) | N/A | 3.1% |
Aspiration alone (comparison group) | 82.3% (TICI 2b/3) | N/A | N/A |
Note: These results highlight the importance of balancing radial force to achieve both effective clot removal and vessel wall safety in stroke interventions.
Design Strategies
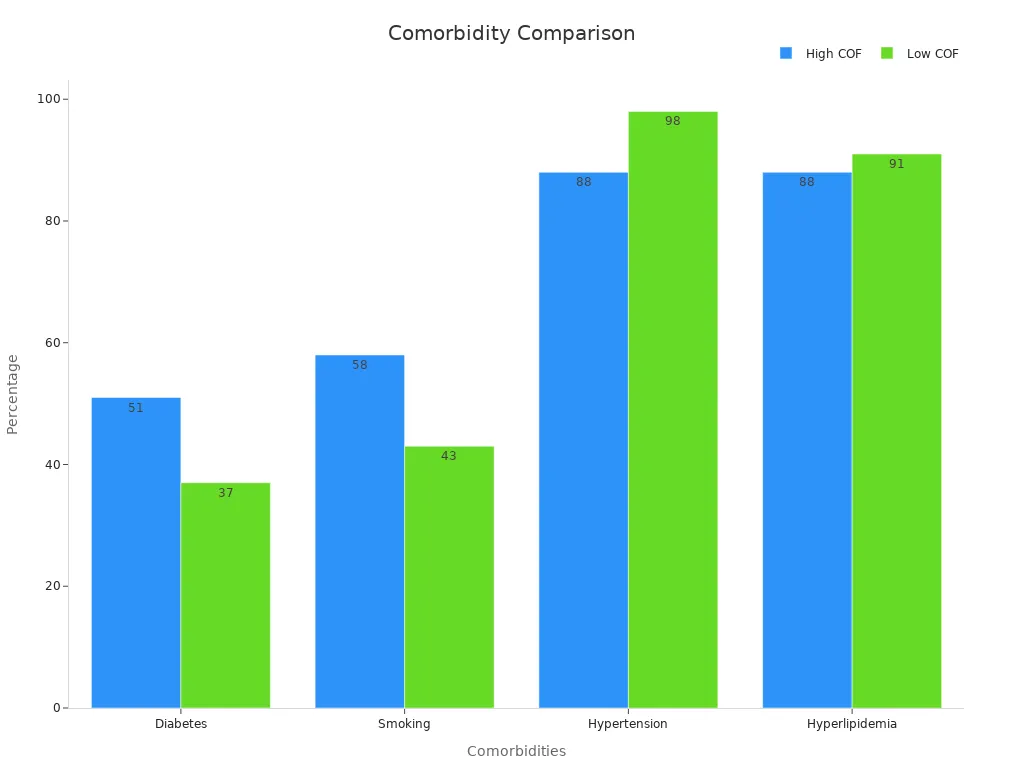
Material and Geometry
Stent design relies on careful selection of materials and geometric features to optimize chronic outward force (COF). Engineers often choose nitinol for its superelasticity and shape memory, which help maintain vessel patency during and after thrombectomy. Adjusting strut thickness and mesh cell shape can directly influence radial resistance and hoop force. For example, reducing strut thickness from 150 µm to 100 µm preserves radial strength but lowers strain on the vessel wall. This adjustment decreases the risk of late-stent thrombosis and myocardial infarction. Clinical data show that strut thicknesses above 100 µm increase adverse events, so designers aim for thinner struts without sacrificing support.
Multi-objective optimization studies confirm that changes in geometry, such as arc structures and mesh size, improve both flexibility and clot capture. Experimental tests using vascular models demonstrate that optimized stent retrievers remove clots more efficiently and safely. The self-expanding stent design, which adapts to vessel contours, further enhances performance by maintaining consistent outward force.
Design Principle / Variable | Supported Numerical Evidence and Advantages | Challenges / Considerations |
|---|---|---|
Proximal Flow Arrest (BGC use) | Zero thrombus migration, reduced procedural time, 100% technical success rate | Operator experience required, higher initial device cost |
One-Stage Operation | Streamlined procedure, lower complication risk | Riskier in patients with large infarct cores |
Procedure Success Rate | 100% technical success, improved clinical outcomes | Dependent on operator skill and anatomy |
Procedure Adaptability | Adaptable to various anatomies | Tailored approaches increase complexity |
Risk Mitigation | Embolic protection, reduced stroke progression risk | Benefits depend on operator experience |
Cost-Effectiveness | Cost savings from reduced time and complications | Higher initial equipment costs |
Surface Treatments
Surface treatments play a vital role in stent safety and effectiveness. Drug-eluting coatings release medications that inhibit cell proliferation, reducing the risk of in-stent restenosis. Comparative studies show that drug-eluting stents lower restenosis rates and improve patient prognosis compared to bare-metal stents. Surface functionalization strategies, such as ultra-hydrophilic coatings, promote endothelial repair and reduce neointimal hyperplasia. Quantitative data reveal that ultra-hydrophilic surfaces achieve a 1.5- to 3-fold reduction in intimal hyperplasia compared to baseline, with similar early healing as bare-metal stents.
Parameter | Ultra-Hydrophilic Surface (UHS) | Bare Metal Stents (BMS) | Drug-Eluting Stents (DES) | Statistical Significance (p-value) |
|---|---|---|---|---|
Reduction in intimal hyperplasia | 1.5- to 3-fold reduction | Baseline | Baseline | p < 0.04 |
Endothelialization (early healing) | Similar to BMS | Baseline | Lower | Not specified |
Thrombotic indices | Rare or none | Rare | Most frequent | p < 0.01 |
Uncoated stents also show greater endothelialization than some polymer-coated options, supporting the need for careful selection of surface treatments. By combining optimized material, geometry, and surface properties, stent designers can balance radial force for effective clot removal while minimizing vessel injury.
High-radial-force nitinol tubing gives thrombectomy stents the strength to engage clots and restore blood flow. However, finding the right balance remains essential. Devices with excessive radial force can increase neointimal proliferation and restenosis, as shown in long-term studies.
Aspect | High Radial Force Stents | Low Radial Force Stents |
|---|---|---|
Restenosis Rate | Higher | Lower |
Vessel Patency | Reduced | Improved |
Lumen Loss | Increased | Less |
Ongoing advances in stent design and material science continue to improve patient outcomes and safety.
FAQ
What is high-radial-force nitinol tubing?
High-radial-force nitinol tubing refers to a nickel-titanium alloy tube designed to push outward with significant strength. This property helps thrombectomy stents grip and remove blood clots while maintaining flexibility inside blood vessels.
Why does radial force matter in thrombectomy stents?
Radial force allows the stent to press against the clot and vessel wall. This action secures the clot for removal and helps restore blood flow. Proper radial force improves treatment success and reduces the risk of complications.
Can high radial force cause vessel injury?
Excessive radial force may increase the risk of vessel wall injury, such as thickening or loss of elasticity. Device designers aim to balance force for effective clot removal while protecting the vessel.
How do surface treatments improve stent safety?
Surface treatments, such as drug-eluting or ultra-hydrophilic coatings, help reduce cell overgrowth and promote healing. These coatings lower the risk of restenosis and improve long-term vessel patency.
See Also
The Importance Of Nitinol Tubing In Minimally Invasive Surgery
How Nitinol Tubing Drives Progress In Medical Technology
Nitinol Tubing’s Critical Role In Cutting-Edge Medical Uses
The Impact Of Nitinol Tubing On Modern Medical Devices
The Process Behind Manufacturing Nitinol Tubing For Medicine

