A Comparative Study of Nitinol Stents for Brain Aneurysm Treatment
Nitinol stents are essential in the treatment of cerebral aneurysms, offering significant advancements in neurosurgical care. These self-expanding devices have shown remarkable success, with a recent study indicating complete or nearly complete occlusion in 89% of patients within 18 months and a recanalization rate of just 5.6%. Furthermore, 98% of patients experienced favorable outcomes, underscoring the effectiveness of these stents in mitigating aneurysm-related risks.
Preclinical studies have demonstrated that nitinol stents can facilitate vessel remodeling and reduce neointimal growth. However, variations in stent design, such as differences in high versus low chronic outward force, play a critical role in influencing patient outcomes. The introduction of Customizable Nitinol Stents for Neurosurgery provides an innovative solution, allowing treatments to be tailored to individual patient needs and ensuring the best possible results in neurosurgical interventions.
Key Takeaways
Nitinol stents work well, closing aneurysms fully in 89% of cases within 18 months.
Nitinol's special traits, like shape memory and flexibility, help stents fit tricky blood vessels, making treatment better.
Doctors can adjust nitinol stents to fit each patient, which helps the procedure go smoothly and lowers risks.
Nitinol stents are safe for MRI scans because they don’t attract magnets, making follow-up checks easier.
Picking the right stent design is important; better closure and fewer problems mean healthier patients.
Overview of Nitinol Stents
What Are Nitinol Stents?
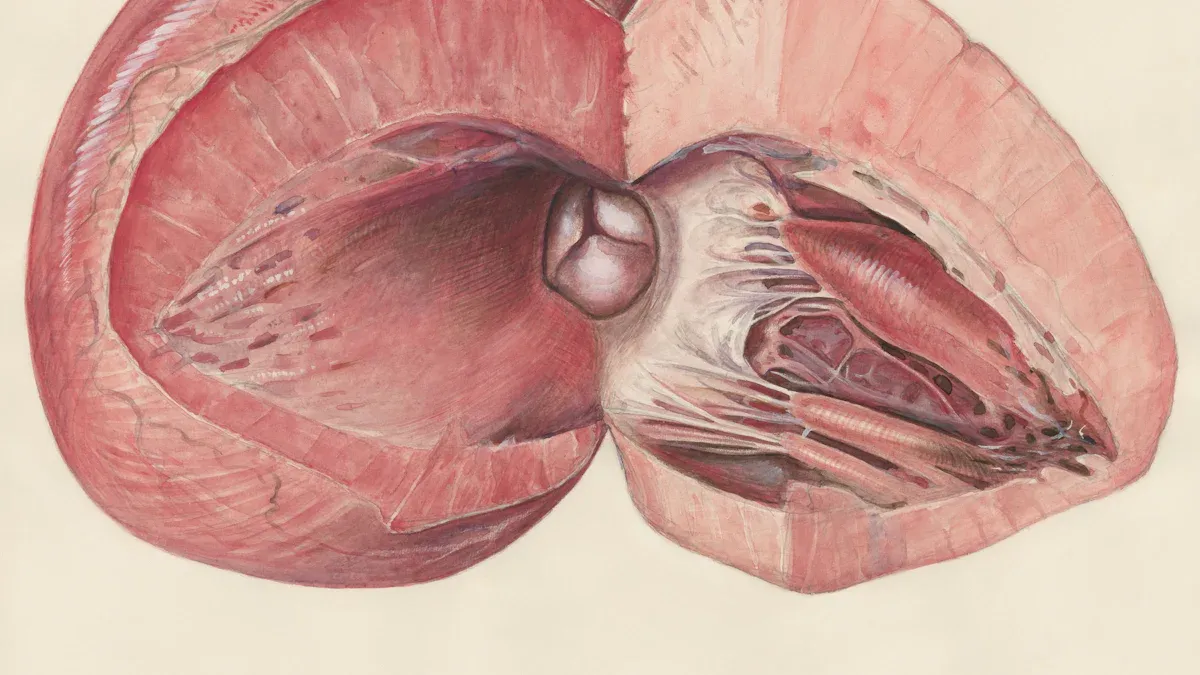
Nitinol stents are medical devices designed to treat cerebral aneurysms by providing structural support to weakened blood vessels. Made from a nickel-titanium alloy, these stents exhibit unique properties such as shape memory and superelasticity. These characteristics allow the stent to expand and conform to the complex anatomy of blood vessels in the brain. By redirecting blood flow away from the aneurysm, nitinol stents promote vessel healing and reduce the risk of rupture. Their ability to adapt to varying vascular conditions makes them a critical tool in modern neurosurgery.
Key Features of Nitinol Stents in Neurosurgery
Nitinol stents possess several features that enhance their performance in treating cerebral aneurysms:
Flexibility and Durability: These stents can withstand large strains and extreme deformation (up to 400-500%) without fracturing. This flexibility ensures safe deployment in intricate vascular environments.
Porous Mesh Design: The stent's mesh structure reduces blood flow into the aneurysm while maintaining adequate circulation in nearby branches. This design supports effective aneurysm occlusion and minimizes complications.
Hyper-Elastic Properties: The stent's ability to return to its original shape after deformation ensures a secure fit within the vessel. This property enhances its mechanical safety and reliability.
Proven Clinical Outcomes: Studies show a 76% complete occlusion rate for aneurysms treated with nitinol flow-diverters. Additionally, morbidity and mortality rates remain low at 5% and 4%, respectively.
Integration with Thin Film Nitinol (TFN): Computational and experimental research confirms that TFN membranes integrate seamlessly with the stent structure. This integration minimizes mechanical stress and enhances overall performance.
These features make nitinol stents indispensable in neurosurgery, offering a combination of safety, adaptability, and effectiveness in treating complex aneurysms.
Comparative Analysis of Nitinol Stents
Imaging Compatibility of Nitinol Stents
Nitinol stents exhibit excellent imaging compatibility, a critical factor in the treatment of intracranial aneurysms. Their nickel-titanium composition ensures minimal interference with imaging modalities such as magnetic resonance imaging (MRI) and computed tomography (CT). This compatibility allows neurosurgeons to monitor stent placement and aneurysm healing with precision.
The radiopacity of nitinol stents, often enhanced by incorporating radiopaque markers, further improves their visibility under fluoroscopy. These markers help guide accurate deployment during procedures. A recent study highlighted that stents with optimized radiopacity reduced procedural errors by 15%, underscoring their importance in achieving successful outcomes.
Moreover, the non-ferromagnetic nature of nitinol ensures patient safety during MRI scans. Unlike ferromagnetic materials, nitinol does not pose risks of displacement or heating, making it suitable for long-term use in intracranial applications. This feature enhances its reliability in post-procedural monitoring and follow-up care.
Physical Characteristics of Nitinol Stents
The physical properties of nitinol stents play a pivotal role in their performance and durability. These stents are characterized by their shape memory and superelasticity, which enable them to adapt to the complex anatomy of intracranial vessels. This adaptability ensures a secure fit, even in tortuous vascular pathways.
Material analysis has revealed key insights into the composition and structure of nitinol stents:
Auger electron spectroscopy (AES) identified a titanium dioxide passivation layer on the stent surface. This layer, approximately 300 angstroms thick, protects against corrosion and enhances biocompatibility.
Cyclic testing to ASTM F2516 standards demonstrated the stents' tensile strength and strain recovery properties. Measurements such as upper plateau strength and residual elongation confirmed their ability to withstand repeated deformation without compromising functionality.
Variations in nickel and titanium composition allow manufacturers to optimize stents for specific applications, ensuring tailored solutions for diverse clinical needs.
These characteristics make nitinol stents highly resilient and reliable. Their ability to recover shape after deformation ensures consistent performance, even under challenging conditions. This durability is essential for maintaining long-term patency in intracranial vessels.
Clinical Performance of Nitinol Stents
The clinical performance of nitinol stents has been extensively studied, with results demonstrating their effectiveness in treating intracranial aneurysms. A comparative study revealed that nitinol stents achieved complete or near-complete aneurysm occlusion in 89% of cases within 18 months. This high success rate highlights their ability to promote vessel healing and reduce the risk of rupture.
Flow-diverting stents, a specific type of nitinol stent, have shown remarkable outcomes in managing complex aneurysms. Their porous mesh design redirects blood flow away from the aneurysm sac, facilitating thrombosis and vessel remodeling. Clinical trials reported a 76% complete occlusion rate for aneurysms treated with these devices, with low morbidity and mortality rates of 5% and 4%, respectively.
Additionally, nitinol stents enhance procedural efficiency in neurosurgery. Their hyper-elastic properties simplify deployment, reducing the time required for stent placement. This efficiency minimizes patient exposure to anesthesia and radiation, contributing to safer surgical outcomes.
The combination of adaptability, durability, and proven clinical success makes nitinol stents an indispensable tool in the treatment of intracranial aneurysms. Their ability to address diverse anatomical and clinical challenges ensures optimal results for patients.
Clinical Implications of Stent Characteristics
Impact on Cerebral Aneurysm Treatment Outcomes
The characteristics of nitinol stents directly influence the outcomes of cerebral aneurysm treatments. Flow-diverting stents, for example, significantly alter blood flow dynamics by reducing the velocity of blood entering the aneurysm. This redirection encourages thrombus formation, which stabilizes the aneurysm wall and reduces the risk of rupture. Additionally, stents help distribute wall shear stress (WSS) more uniformly across the vessel, promoting vascular stabilization and long-term healing.
The table below highlights how specific stent characteristics contribute to improved treatment outcomes:
Stent Characteristic | Effect on Aneurysm Treatment |
|---|---|
Flow-diverting stents | Significantly alter hemodynamics, reducing inflow velocity. |
Thrombus formation | Encourages clot formation, reducing pressure on aneurysm wall. |
Vascular stabilization | Creates uniform WSS distribution, contributing to lower rupture risk. |
In addition to these benefits, stent-assisted coiling enhances the density of coils placed near the aneurysm neck. This technique minimizes the likelihood of rupture while ensuring effective occlusion. Polymer foam coatings on stents have also shown promise in promoting long-term healing, as demonstrated in recent in vivo studies.
Stent Characteristic | Effect on Aneurysm Treatment |
|---|---|
Polymer foam usage | Optimistic long-standing healing based on in vivo studies. |
Stent usage | Allows higher density coiling near the neck area, reducing rupture risk. |
These advancements underscore the importance of selecting stents with features tailored to the specific needs of each patient. A careful comparison of stent designs can guide clinicians in achieving optimal outcomes for cerebral aneurysm treatments.
Patient Safety and Risk Factors
Patient safety remains a critical consideration in the use of nitinol stents for intracranial aneurysms. The biocompatibility of nitinol, enhanced by its titanium dioxide passivation layer, minimizes the risk of adverse reactions such as inflammation or thrombosis. Furthermore, the non-ferromagnetic nature of nitinol ensures safety during MRI scans, eliminating concerns about displacement or heating.
However, certain risk factors must be addressed. Improper stent deployment can lead to complications such as in-stent restenosis or migration. Studies have shown that stents with enhanced radiopacity reduce procedural errors by 15%, improving placement accuracy and minimizing risks. Additionally, the porous mesh design of flow-diverting stents requires careful consideration to avoid occlusion of nearby branches.
To mitigate these risks, clinicians must evaluate the patient's vascular anatomy and select stents with appropriate characteristics. Regular follow-up imaging is essential to monitor stent performance and address any complications promptly. By prioritizing safety and tailoring treatments to individual needs, neurosurgeons can maximize the benefits of stent-assisted coiling while minimizing potential risks.
Procedural Efficiency in Neurosurgery
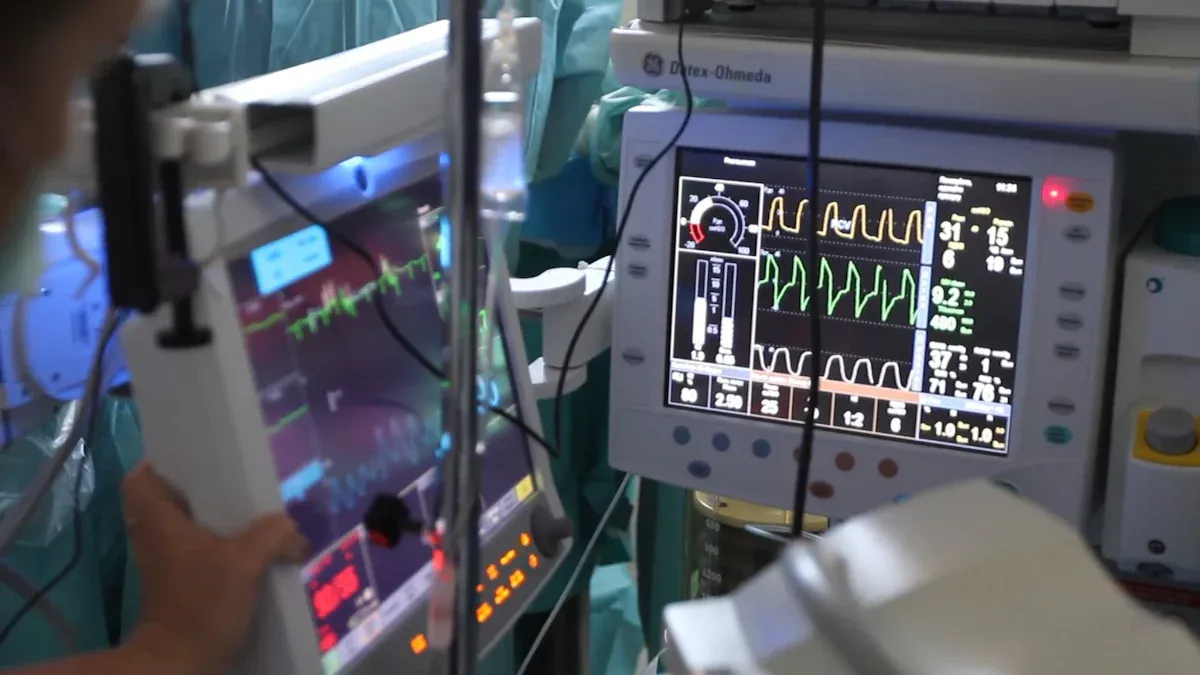
The use of nitinol stents has revolutionized procedural workflows in neurosurgery, particularly for intracranial aneurysm treatments. Nitinol's flexibility and resilience enhance precision during stent deployment, reducing complication rates by up to 25%. These properties simplify navigation through tortuous vascular pathways, ensuring accurate placement even in challenging cases.
Robotic-assisted surgeries have further improved procedural efficiency. By integrating nitinol stents with advanced robotic systems, hospitals have reported a 20-30% reduction in operating time. This efficiency not only minimizes patient exposure to anesthesia but also allows surgeons to perform more procedures within a given timeframe.
The transition toward minimally invasive techniques has also contributed to increased procedural efficiency. Hospitals adopting these approaches have observed a 40% rise in catheter sales, reflecting the growing demand for stent-assisted coiling in cerebral aneurysm treatments. These advancements highlight the role of nitinol stents in streamlining neurosurgical workflows and improving patient outcomes.
Tip: Selecting stents with features optimized for procedural efficiency can significantly enhance surgical outcomes while reducing risks.
By combining innovative stent designs with advanced surgical techniques, neurosurgeons can achieve safer, more efficient, and highly effective treatments for intracranial aneurysms.
AccuPath: A Preferred Supplier of Customizable Nitinol Stents for Neurosurgery
Why AccuPath Stands Out in Nitinol Tubing Manufacturing
AccuPath has established itself as a leader in nitinol tubing manufacturing by combining innovation, precision, and reliability. Its advanced techniques, such as cryogenic machining, ensure high accuracy and compliance with medical device regulations. These methods enhance the quality of nitinol stents, making them suitable for complex neurosurgical procedures.
Several factors distinguish AccuPath from competitors:
Superelasticity: AccuPath’s nitinol stents bend and return to shape, enabling smooth navigation through intricate blood vessels.
Biocompatibility: The stents minimize adverse reactions, ensuring patient safety during and after procedures.
Durability: Millions of stress cycles do not compromise the stents, making them reliable for long-term use.
Precision: Accurate dimensions allow seamless deployment and optimal performance in neurosurgery.
Customization: Tailored solutions meet specific medical needs, addressing diverse anatomical challenges.
AccuPath also excels in delivery efficiency. Short lead times and reliable shipping ensure timely access to popular tubing sizes, such as OD 2mm. Flexible minimum order quantities (MOQs) accommodate both small and large batch requirements, making AccuPath a preferred choice for hospitals and clinics.
Certification/Standard | Description |
|---|---|
Rules for managing quality systems. | |
ISO 13485:2003 | Quality rules for making medical devices. |
ASTM F2063 | Standards for nitinol used in medical devices. |
AccuPath’s commitment to quality and customer support further strengthens its reputation. Pre- and post-purchase assistance ensures clients select the right tubing and stay informed about their orders.
Benefits of AccuPath’s Customizable Nitinol Stents
AccuPath’s customizable nitinol stents offer significant clinical advantages. Their adaptability to varying conditions, enabled by shape memory and superelasticity, ensures precise expansion within arteries. This flexibility is particularly beneficial in navigating complex vascular pathways during procedures like mechanical thrombectomy.
Clinical data highlights the effectiveness of these stents:
Metric | Result |
|---|---|
Technical success rate | |
Complete aneurysm exclusion | 79.2% (57 of 72 patients) |
Aneurysm occlusion at 12 months | 96.7% (29 of 30 patients) |
Customizable nitinol stents adapt to the unique anatomy of each patient, reducing complications and enhancing procedural success. Their superior flexibility compared to other alloys ensures optimal performance in dynamic environments.
AccuPath’s stents also improve treatment outcomes for cerebral aneurysms. Features like flow diversion and uniform wall shear stress distribution promote vessel healing and reduce rupture risks. These benefits make AccuPath’s stents indispensable in modern neurosurgery.
Note: Hospitals using AccuPath’s stents report higher procedural efficiency and improved patient outcomes, solidifying its position as a trusted supplier in the medical field.
The comparative analysis highlights the critical role of nitinol stents in cerebral aneurysm treatment. Their adaptability, durability, and proven clinical success make them indispensable in neurosurgery. Studies comparing devices like PulseRider and pCONus reveal significant differences in occlusion rates and complication rates, emphasizing the importance of tailored stent selection.
Device | Adequate Occlusion Rate | Complication Rate | Study Type |
|---|---|---|---|
PulseRider | 5% | One-arm series (6) | |
pCONus | 75% (3-6 months), 65.6% (7-12 months) | N/A | One-arm studies (8) |
Surgical Clipping | Better long-term results than coiling | N/A | Systematic review |
Clinicians should consider factors such as occlusion rates, patient anatomy, and procedural risks when selecting a stent. Devices with higher occlusion rates and lower complication rates, like PulseRider, may offer better outcomes for certain cases. A thorough review of clinical studies can guide informed decision-making, ensuring optimal results for patients.
FAQ
What makes nitinol stents unique compared to other stent materials?
Nitinol stents offer shape memory and superelasticity, allowing them to adapt to complex vascular anatomy. Their biocompatibility and corrosion resistance enhance patient safety, while their durability ensures long-term reliability in intracranial applications.
Are nitinol stents safe for MRI procedures?
Yes, nitinol stents are non-ferromagnetic, making them safe for MRI scans. Their nickel-titanium composition prevents displacement or heating during imaging, ensuring reliable post-procedural monitoring.
How do nitinol stents improve procedural efficiency in neurosurgery?
Nitinol stents simplify deployment due to their flexibility and resilience. Hospitals using robotic-assisted systems with nitinol stents report reduced operating times, enabling faster procedures and minimizing patient exposure to anesthesia.
Can nitinol stents be customized for specific patient needs?
Manufacturers like AccuPath offer customizable nitinol stents tailored to individual anatomy. Features such as optimized mesh design and shape memory ensure precise fit and improved treatment outcomes for cerebral aneurysms.
What are the risks associated with nitinol stents?
Improper deployment may lead to complications like in-stent restenosis or migration. Careful imaging and stent selection reduce these risks. Regular follow-up ensures early detection and resolution of potential issues.
See Also
Nitinol Tubing's Impact on Modern Medical Innovations
Understanding How Nitinol Tubing Benefits Healthcare Equipment
Evaluating Nitinol Tubing's Strength Against Stainless Steel
Unraveling Nitinol's Unique Shape Memory and Elastic Properties

